Published: April 3, 2024
5 Ways to Stop Plantar Fasciitis in Its Tracks
By: N. Jake Summers, DPM, FACFAS of Elliot Orthopaedic Surgery Specialists
As the chill of winter melts away and the warmth of spring calls us outdoors, many of us are excited to get outside and resume warm weather activities. However, amidst the excitement of returning to exercise, there lurks a common adversary: plantar fasciitis. As a foot and ankle surgeon, I've witnessed firsthand how the transition from winter hibernation to spring activity can trigger painful flares of heel discomfort and plantar fasciitis in many individuals. In fact, during this time of year it is one of the most common complaints seen in the office.
 What is Plantar Fasciitis?
What is Plantar Fasciitis?
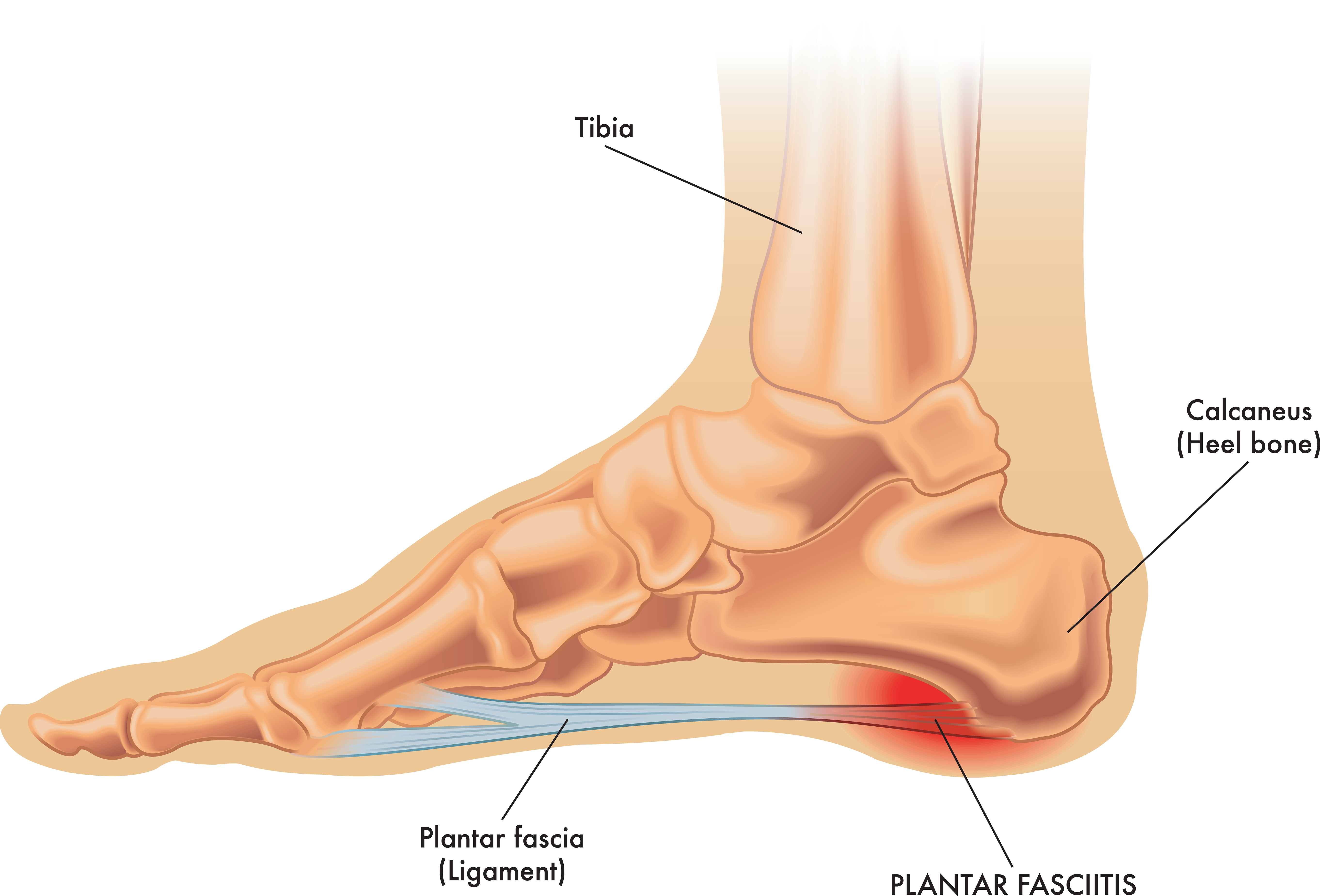
Plantar fasciitis is characterized by inflammation of the thick band of ligament (the plantar fascia) that runs across the bottom of your arch originating from your heel. It often manifests as stabbing pain near the heel, particularly with the first steps in the morning or after prolonged periods of rest. While the exact cause can vary from overuse to poor footwear choices, one of the most common causes is actually from lack of stretching/flexibility of the Achilles tendon and calf muscles, leading to tension and stress on the plantar fascia. The sudden increase in peoples’ activity levels as spring arrives is a prime culprit for exacerbating this condition.
How Can I Prevent Plantar Fasciitis?
As we lace up our running shoes and hit the pavement, let’s take preventive measures that can help lower the risk of developing or worsening plantar fasciitis:
1. Proper Footwear Selection: Invest in supportive shoes specifically designed for your chosen activity. Look for options with adequate arch support, cushioning, and a firm heel counter to minimize strain on the plantar fascia.
2. Gradual Progression: Avoid the temptation to dive headfirst into intense workouts after a period of inactivity. Instead, gradually increase the duration and intensity of your exercise regimen to allow your feet time to adapt and strengthen gradually. Alternating days between weight bearing exercises and non-weight bearing exercises can also be helpful.
inactivity. Instead, gradually increase the duration and intensity of your exercise regimen to allow your feet time to adapt and strengthen gradually. Alternating days between weight bearing exercises and non-weight bearing exercises can also be helpful.
3. Stretching and Strengthening Exercises: Incorporate regular stretching and strengthening exercises into your routine to improve flexibility and stability in the muscles and ligaments surrounding the foot. Focus on calf stretches, toe curls, and towel scrunches to target the plantar fascia and its supporting structures. Deep tissue massage and manual stretching of the arch and plantar fascia can also be helpful.
4. Weight Management: Excess body weight can increase strain on the feet and exacerbate plantar fasciitis symptoms. Maintaining a healthy weight can alleviate undue stress on the plantar fascia and promote overall foot health. As we focus on losing weight, including lower impact weight training and cardio such as cycling/stationary bikes can be a good place to begin.
5. Orthotic Support: Consider using pre-fabricated orthotics or shoe inserts to provide additional support and cushioning for your feet. These devices can help redistribute pressure and correct biomechanical imbalances that contribute to plantar fasciitis. There is a plethora of pre-fabricated orthotics available, and many may not be helpful. Local running stores will typically have appropriate selections and staff that may be able to provide advice when seeking orthotics.
Learn about Elliot Orthopaedic Surgery Specialists
What Are the Plantar Fasciitis Treatment Options?
While prevention is paramount, it's equally essential to address plantar fasciitis promptly if symptoms arise. Treatment options may include:
Rest and Ice: The classic frozen water bottle to reduce inflammation and provide a gentle stretch to the arch and plantar fascia is a tried-and-true method. Altering activities to include lower impact exercises during this rest period can be very helpful. Repetitive high impact activity may exacerbate the problem. Yoga or alternative stretching exercises is a great way to remain active and fit while trying to rest and recover from plantar fasciitis.
Anti-inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen can provide relief from pain and reduce inflammation.
Physical Therapy: A tailored physical therapy program focusing on stretching, strengthening, and biomechanical correction can help address underlying imbalances and promote long-term recovery. Physical therapy is one of the most effective ways to recover from plantar fasciitis and to reduce the risk of its recurrence.
Steroid Injections: In some cases, corticosteroid injections may be recommended to provide short-term pain relief for stubborn symptoms. Most people will find relief with a single injection, but some may require a series of injections. Combining this with stretching and strengthening and a good home exercise plan typically provides the best long-term results.
Extracorporeal Shock Wave Therapy (ESWT): This non-invasive treatment utilizes shock waves to stimulate healing and reduce pain in recalcitrant cases of plantar fasciitis.
PRP (Platelet-rich plasma): PRP injections are an alternative to steroid injections and may be a good option for treating recalcitrant cases of plantar fasciitis. They use your own platelets to reduce inflammation and trigger your body’s natural repair and regeneration.
Let’s enjoy the season safely! By incorporating preventive strategies and seeking timely intervention when needed, we can minimize the risk of plantar fasciitis and stride confidently toward a healthier, more active future.
 N. Jake Summers, DPM, FACFAS of Elliot Orthopaedic Surgery Specialists is a podiatric foot and ankle surgeon who has served the southern New Hampshire community since 2016. His practice focuses on ankle joint replacements, foot and ankle deformity correction and reconstruction, sports injuries, trauma, and Charcot reconstruction.
N. Jake Summers, DPM, FACFAS of Elliot Orthopaedic Surgery Specialists is a podiatric foot and ankle surgeon who has served the southern New Hampshire community since 2016. His practice focuses on ankle joint replacements, foot and ankle deformity correction and reconstruction, sports injuries, trauma, and Charcot reconstruction.
You May Also Enjoy:
- The Future of Heart Technology
-
The Power of Tabata: Start Your Fitness Journey with High-Intensity Intervals
